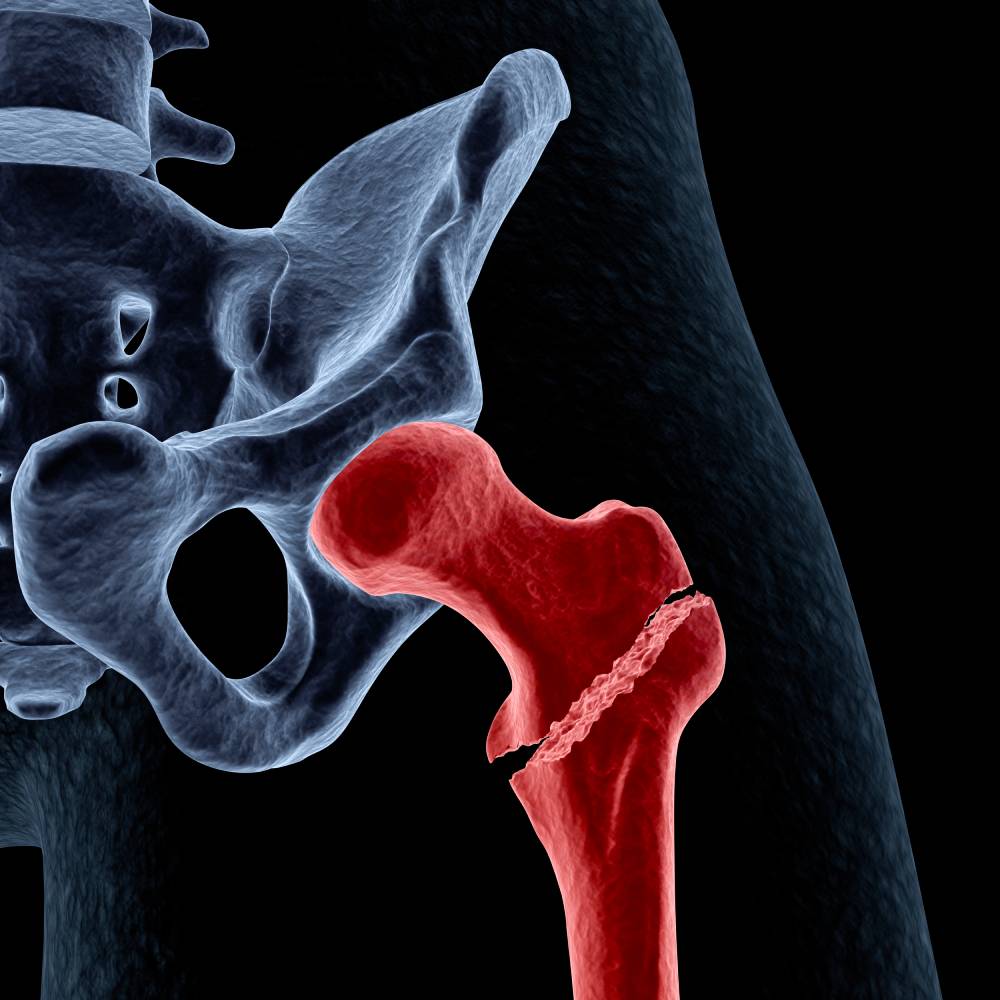
Approximately 10 million people in the U.S. suffer from osteoporosis, a disease that slows the growth of healthy bone and weakens bones over time. Osteoporosis affects nearly 20% of women aged 50 and over and can increase the risk of a fragility fracture during or after joint replacement surgery, of which falling is the most common cause 1. Greater fragility in the bones of a patient with osteoporosis can complicate orthopedic surgery.
Joint replacement is a core type of orthopedic surgery that is affected by osteoporosis. Unfortunately, patients who need joint replacements tend to be older adults who are at greater risk for the disease. In a joint replacement procedure, a worn hip or knee joint is replaced with an implant made of body-safe metal. For most patients, the bones on either side of the implant grow onto it over time or are fused to the joint using a cement-like compound. However, osteoporosis weakens the bones, which may result in poor or no grafting of surrounding bone to the implant. Fragility fractures can also occur during surgery if the surrounding bone is too brittle to withstand manipulation or surgical cutting. Fragility fractures can result in immobility, pain, and an increased risk of complications ranging from infection to death. Most patients who experience this need an urgent revisional surgery, which is complex and should only be performed by experienced clinicians. In addition, if a patient with osteoporosis falls after a knee or hip replacement, even several years after surgery, the weakened bones near their implant can easily break.
In order to improve outcomes, all patients must take deliberate precautions to avoid falling following knee or hip replacement surgery. Osteoporosis patients can also take steps to improve their bone health, whether or not they require or have recently had orthopedic surgery.
Since vitamin D deficiency is common among patients undergoing joint arthroplasty, vitamin D supplements can help improve outcomes. Both bisphosphonates and teriparatide may also improve osteointegration in patients undergoing non-cemented joint arthroplasty 3.
Other beneficial steps include taking calcium supplements, doing bone-loading exercises, fall-proofing one’s home, and wearing well-fitted shoes 2. Focusing on bone health perioperatively can help support better outcomes for orthopedic surgery in patients with osteoporosis 3.
A recent study sought to assess a novel, simple screening protocol to identify orthopedic surgical patients for preoperative dual-energy x-ray absorptiometry 4. Data revealed that a simple screening protocol was able to identify orthopedic surgical candidates at risk of clinical osteoporosis with high sensitivity. However, the proposed screening protocol represents only the very first step of a larger scale bone health optimization initiative.
The development and implementation of a framework for the diagnosis and treatment of patients with decreased bone mineral density is critical to ensuring the best outcomes for patients. One research study recently assessed a large volume of empirical data, synthesizing it succinctly to this end with the incorporation of both a diagnosis algorithm and treatment profile table 5. Using existing tools and future advancements in the field, orthopedic surgeons should be able to take on a more active role in their patients’ bone health and ensure optimal patient outcomes across clinical contexts.
References
1. Does Osteoporosis Run in Your Family? | CDC. Available at: https://www.cdc.gov/genomics/disease/osteoporosis.htm. (Accessed: 3rd June 2023)
2. How does osteoporosis affect knee and hip replacements? Available at: https://utswmed.org/medblog/knee-hip-replacement-osteoporosis/. (Accessed: 3rd June 2023)
3. Russell, L. A. Osteoporosis and orthopedic surgery: effect of bone health on total joint arthroplasty outcome. Curr. Rheumatol. Rep. 15, (2013).
4. Chang, E. et al. A Novel Osteoporosis Screening Protocol to Identify Orthopedic Surgery Patients for Preoperative Bone Health Optimization. Geriatr. Orthop. Surg. Rehabil. 13, (2022). doi: 10.1177/21514593221116413
5. Farmer, R. P. et al. Osteoporosis and the orthopaedic surgeon: basic concepts for successful co-management of patients’ bone health. Int. Orthop. 38, 1731 (2014). doi: 10.1007/s00264-014-2317-y.