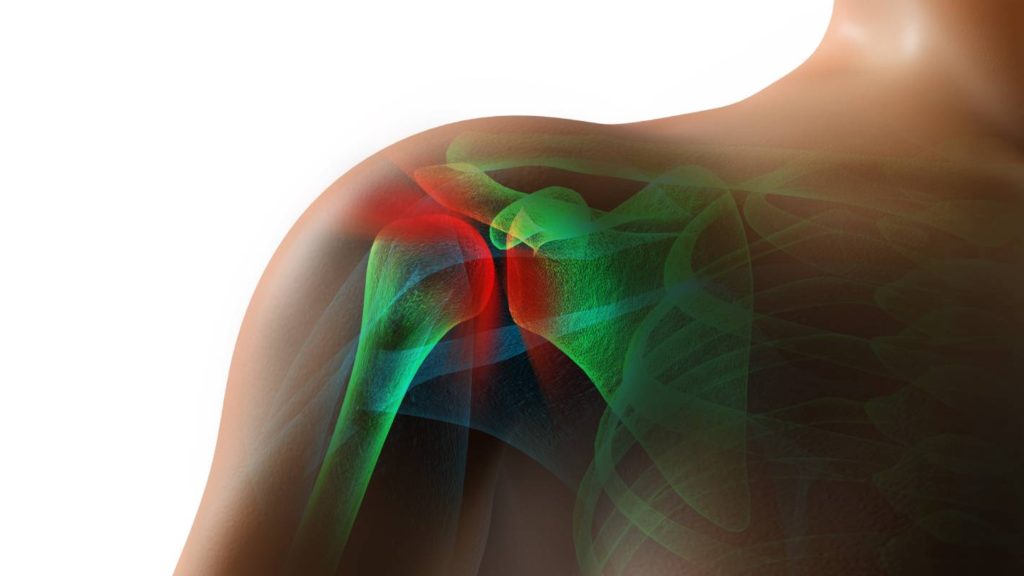
With as many as 70% of patients reporting severe postoperative pain following this operation, arthroscopic shoulder surgery poses a significant challenge to anesthesiologists [1]. It is one of the most painful surgeries, with its associated pain intensity rivaling that of thoracotomies and revision hip and knee arthroplasties [2]. Postoperative pain following shoulder surgery is especially difficult to treat because it resists easy management by anesthetics and nerve blocks [1]. If treated unsuccessfully, it can derail rehabilitation and postpone recovery [1]. While researchers have investigated alternative treatments, the ideal strategy for anesthesia during shoulder surgery is still uncertain.
Currently, the interscalene brachial plexus block (ISB) is one of the most effective anesthesia techniques available for arthroscopic shoulder surgery [1]. Several studies affirm the ISB’s ability to reduce postoperative pain and encourage early recovery [1]. Unfortunately, the ISB is invasive and is associated with phrenic nerve block, potentially leading to several adverse respiratory side effects, such as phrenic nerve palsy, rebounding pain, and nerve block failure [1, 3]. While the rate of complication for the ISB may not be as high as previously reported, transient problems such as paresthesias and dysethesias still occur at significant frequencies, suggesting that the ISB is not an appropriate anesthetic technique in all cases [4]. Therefore, anesthesiologists should look to other approaches when the ISB may be especially risky for their patients.
One such alternative technique is the posterior suprascapular block. Because it occurs more distally along the brachial plexus than the ISB, the suprascapular block can avoid undesirable effects on the phrenic nerve [5]. However, when block location is more distal, clinicians risk administering inferior analgesia [5]. To determine whether the posterior suprascapular block can avoid the side effects associated with ISB while providing adequate analgesia, Lee et al. followed 61 arthroscopic cuff repair patients [1]. Along with the ISB and the suprascapular nerve block, the researchers considered the comparative effects of the axillary nerve block as well [1]. While the posterior suprascapular block was a satisfactory anesthetic choice from four to twenty-four hours following surgery, its inferiority during the first four postoperative hours could significantly delay patient discharge [1, 3]. As a result, it is may not be an adequate replacement for the ISB.
Supraclavicular blocks have also been considered as replacements for the ISB, given their distance from the phrenic nerve [5]. To assess the analgesic efficacy of the supraclavicular block compared to the ISB, Auyong et al. conducted a double-blind trial following 189 shoulder surgery patients [5]. Despite its decreased rate of complications, the researchers observed that the supraclavicular block proved inferior in terms of analgesia, with the supraclavicular group’s average pain scores coming in significantly higher than the ISB group’s [5].
During the same experiment, the researchers also analyzed the analgesic capacities of the anterior suprascapular block [5]. They found it to be noninferior to the ISB [5]. In 2018, Siegenthaler et al. detailed “a proximal ultrasound-guided selective anterior suprascapular nerve block within the supraclavicular fossa,” the anticipated benefit of this technique being minimized risk of phrenic nerve damage with preserved analgesic function [5, 6]. Along with the Auyong et al. experiment, Abdallah et al. also supported Siegenthaler’s positive view of this technique [3]. Their results suggested that anterior suprascapular nerve blocks “consistently block the superior trunk and brachial plexus, even when very small local anesthetic volumes are used” [3].
While clinicians would need further research to justify a widespread pivot from ISB, these results are nonetheless encouraging. Because of its observed ability to manage postoperative pain on par with the interscalene plexus block, the suprascapular block may be an adequate and possibly safer anesthetic alternative for arthroscopic shoulder surgery patients.
References
[1] S. M. Lee et al., “Analgesic effectiveness of nerve block in shoulder arthroscopy: Comparison between interscalene, suprascapular and axillary nerve blocks,” Knee Surgery, Sports Traumatology, Arthroscopy, vol. 20, p. 2573-2578, March 2012. [Online]. Available: https://doi.org/10.1007/s00167-012-1950-5.
[2] D. Q. Tran et al., “Diaphragm-sparing nerve blocks for shoulder surgery, revisited,” Regional Anesthesia & Pain Medicine, vol. 45, no. 1, p. 73-78, January 2020. [Online]. Available: https://doi.org/10.1136/rapm-2019-100908.
[3] F. W. Abdallah et al., “Subomohyoid Anterior Suprascapular Block versus Interscalene Block for Arthroscopic Shoulder Surgery: A Multicenter Randomized Trial,” Pain Medicine, vol. 132, p. 839-853, April 2020. [Online]. Available: https://doi.org/10.1097/ALN.0000000000003132.
[4] A. Bourgeat et al., “Acute and Nonacute Complications Associated with Interscalene Block and Shoulder Surgery: A Prospective Study,” Anesthesiology, vol. 95, p. 875-880, October 2001. [Online]. Available: https://doi.org/10.1097/00000542-200110000-00015.
[5] D. B. Auyong et al., “Comparison of Anterior Suprascapular, Supraclavicular, and Interscalene Nerve Block Approaches for Major Outpatient Arthroscopic Shoulder Surgery: A Randomized, Double-blind, Noninferiority Trial,” Anesthesiology, vol. 129, p. 47-57, July 2018. [Online]. Available: https://doi.org/10.1097/ALN.0000000000002208.
[6] A. Siegenthaler et al., “Ultrasound-Guided Suprascapular Nerve Block, Description of a Novel Supraclavicular Approach,” Regional Anesthesia & Pain Medicine, vol. 37, no. 3, p. 325-328, May-June 2012. [Online]. Available: https://doi.org/10.1097/AAP.0b013e3182409168.